
 Irritable Bowel Syndrome or IBS as it’s commonly called, may not be the most exciting topic to read about. But for the 5 million Canadians who suffer from it, learning about breakthroughs in treatment is definitely news worth reading. Medical research has made the connection now between IBS and the microbiome, the immune system and the nervous system. While stress and food intake may confound an IBS problem, breakthroughs in our understanding of the microbes in our intestines are helping to solve the deeper issues that can drive this health condition.
Irritable Bowel Syndrome or IBS as it’s commonly called, may not be the most exciting topic to read about. But for the 5 million Canadians who suffer from it, learning about breakthroughs in treatment is definitely news worth reading. Medical research has made the connection now between IBS and the microbiome, the immune system and the nervous system. While stress and food intake may confound an IBS problem, breakthroughs in our understanding of the microbes in our intestines are helping to solve the deeper issues that can drive this health condition.
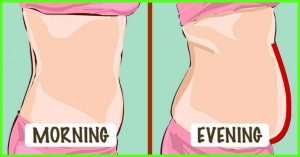
IBS symptoms can include bloating, excess gas and burping, some degree of constipation, diarrhea or both, and often an element of abdominal pain or discomfort. As a naturopathic physician, I regularly treat patients who have been told they have IBS, and that there’s not much they can do about it. The fact is, there are potential solutions to these issues. My first step is to explain that IBS is a diagnosis of exclusion, meaning we must rule out overt infection, cancer, inflammatory bowel disease, reproductive issues and more. Once we’ve done that, we can take steps to find out what is causing that person’s IBS.
Some of my patients respond well to avoiding certain foods, so we usually work to identify food triggers. Some MDs are sharing the research out of Monash University about the FODMAP diet which are foods known to cause IBS symptoms in some people. These foods can provide the fuel to our intestinal bacteria to make gas. But people with a healthy gut can handle those foods just fine, and many FODMAP foods are healthy foods, like broccoli, apples and garlic. If someone feels better on a FODMAP elimination diet, I see that not as a solution, but as a clue that their intestinal microbiome needs work.
By far the most common cause of IBS in my experience is an imbalance in the bacterial lining of the intestines called the microbiome. The large intestine is supposed to have a lot of bacteria and it is normal to ferment the leftover foods there. But the 12 feet of the small intestine are supposed to be relatively bacteria-free. Even if bacteria that is normal to have in the large intestine ends up growing in the small intestine, these bacteria will ferment the normal healthy foods we eat and create gas, intestinal irritation and nutritional issues.
What can cause bacterial overgrowth in the small intestine? There are many factors, but the most common one is a history of gastrointestinal infection. Even a case of traveller’s diarrhea, food poisoning, or viral gastroenteritis that resolves nicely can trigger an autoimmune reaction in about 20% of people. That autoimmune reaction can attack the nerves that stimulate the muscles that cause the sweeping motion inside the small intestine that moves food along between meals. Without this motion, food pools in the small intestine, bacteria can migrate upward from the large intestine, a ‘compost’ is formed, and excess bacteria blooms. Studies of military personal showed that prior gastrointestinal infection was a much stronger predictor of who would get IBS than stress level. Other studies have shown that GI infections can lead to motility disorders in the esophagus and intestines.
Brain injuries are also a potential cause of Small Intestine Bacterial Overgrowth (SIBO). The brain orchestrates the motility of the small intestine, so a brain injury can hamper its ability to coordinate the flushing of the small intestine, allowing a bacterial overgrowth to ensue. Autoimmune disease can also be connected, as well as abdominal surgeries, long term diabetes and more.
Fortunately, there is a specialized test for SIBO that can be ordered through naturopathic physicians. The gold standard test is a series of breath tests that looks for hydrogen and methane gases that have formed in the gut, been absorbed into the blood and are then breathed out. If a test comes back positive, I coach my patients on a four-step program. The first step is to prepare the intestine by opening up the biofilm that the bacteria hide out in. Then we use prescription or herbal antibacterial agents that exclusively target the bacteria in the small intestine. When that phase is complete, patients’ IBS symptoms are significantly better and we work on addressing the underlying cause, which is the motility disorder in the small intestine. There are prescription and herbal “pro-kinetic” agents that rehabilitate the muscles of the inner small intestine so the problem will stay away for good. In addition, we work to heal the intestinal lining to make it more resilient using natural medicines and SIBO specific probiotics.
People who live with IBS deserve to understand why they have these symptoms and what they can do about it. The goal is to repair the gut once and for all, not just manage symptoms. When we understand and treat the underlying issues, lasting resolution is possible.





No comment yet, add your voice below!